
The results of the study indicate that a closer working relationship between the antimicrobial stewardship program and the infection control team pays off in lower incidence of C. diff.

The results of the study indicate that a closer working relationship between the antimicrobial stewardship program and the infection control team pays off in lower incidence of C. diff.
Join us for the inaugural MJH Life SciencesTM COVID-19 Coalition webinar event, “Battling Dual Threats: Flu and COVID-19 Converge,” featuring perspectives across virology and epidemiology.

As these healthcare worker serology studies are designed and performed, we need more insight beyond just PPE use and symptoms, but also internal and external exposures.
Jason Tetro: “There are going to be COVID-19 waves every year. What we hope is that that vaccine is going to be able to help us to be able to have that protection whenever those waves are hitting us.”
It is imperative that infection preventionists engage and combat this messaging on social media and wherever it occurs. To not do so, allows misinformation to fan the pandemic, placing all of our lives at risk.
Infection preventionists need to be able to articulate to those who feel that the young are safe just because their fatality rate is extremely low, that even in this age group there are major concerns regarding long-term consequences of this virus.
J. Hudson Garrett Jr., PhD, MSN, MPH: “I think the role of the infection preventionist has always been of the most critical importance. Every time we have an outbreak or, now, a pandemic, it highlights that further.”

Melinda Benedict, MS, CIC, CFER: “I think for infection preventionists: If you’re not already involved in your endoscopy department or you haven’t been invited in, see if you can get in and just continue to check it out and see what’s going on, especially if the reprocessing and cleaning of the scope is actually done within that clinic.”

Anthony Harris, MD, MBA, MPH: “Really now it’s all about testing. How do we test? What scale do we test with? And, you know, what are the steps toward getting that access to the testing levels that we need necessary to mitigate risk?”
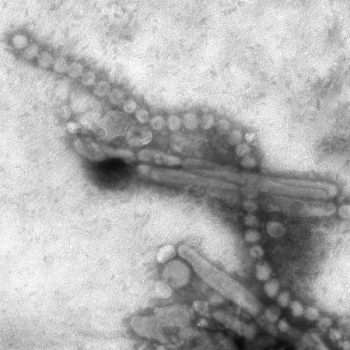
The case involves a 25-year-old Reno man who’d gotten mild symptoms of the disease in April but developed more severe symptoms when he got reinfected in mid-May.

Rebecca Leach, RN, BSN, MPH, CIC: “I’m a very strong vaccine proponent. I do believe in them, and I think they should be mandatory if you’re working in healthcare.”

The CDC released new guidance regarding recommendations for post-exposure COVID-19 testing. Here’s what this means for infection preventionists and public health.

Sharon Ward-Fore, MS, MT(ASCP), CIC: “Practices drift. You can become complacent and maybe your level of awareness has decreased…. So, infection preventionists need to be really aware of what’s happening in the areas they cover as far as PPE usage is concerned.”

If you see something, say something. Let coworkers know when they may have breached infection control practices such as forgetting to wash their hands, not wearing PPE properly, or missed opportunities to clean a high-touch surfaces.

Sharon Ward-Fore, MS, MT(ASCP), CIC: “Although EVS is in charge of the cleaning process infection preventionists work carefully with them to make sure the process is followed by auditing it frequently. And both sides provide feedback to each other just to make sure everything follows best practices.”

Knowing the needs of patients, how can we safely allow visitors again? When will universal masking not be required? A piece to this is that there is no hard rule. These are conversations that require considerable collaboration and plans to scale up and scale down.

Especially in healthcare settings, when infection preventionists need to explain protocols and guidelines to their fellow healthcare workers and patients, something can always be lost in translation if much of the face remains hidden.

Kevin Kavanagh, MD: “Getting this message out is something which we need to do. Infection preventionists can be very, very much instrumental in getting out the correct message and counteracting the false messaging, which we are hearing on both social media and also, unfortunately, from our elected officials.”

Linda Spaulding: “We [infection preventionists] have listening sessions with staff and we talked to them about proper mask wearing 24/7. We can do a listening session and we still have people sitting there with a mask under their nose, while we’re telling them not to. You have to continuously stress this among healthcare workers, be it whatever department.”

Experts discuss the pros and cons of reopening schools.
This year we have to do more than just rely on the flu vaccine. Avoiding the flu plus COVID-19 catastrophe is contingent on the US widely embracing public health guidance of wearing masks, meticulous hand hygiene and social distancing.

Neck gaiters weren’t the only face coverings tested: in all 14 were analyzed, from N95s (unsurprisingly judged to be the most effective in containing COVID-19 spread) to bandanas (not much more effective then neck gaiters, according to the study).

Dalilah Restrepo, MD: “I think now infection preventionists should be part of a school board, should be part of any executive board, of any corporate area, because there is no way that you can expect this expertise to just come about for other folks that aren’t trained in infection prevention.”
One example of a way that IPs can collaborate with other departments to implement a vaccination program is to work with occupational health and emergency response departments to have a mass vaccination drill.

Linda Spaulding, RN, BC, CIC, CHEC, CHOP: “Infection control people really have to monitor closely all respiratory viruses that are out there and be sure that you’re working actively with management to help put in place whatever needs to be put in place.”

Film healthcare workers as they don and doff N95s, show that video to participants (explaining where they got it right, and where they got it wrong), and then have the participants don and doff again with more input from trainers.
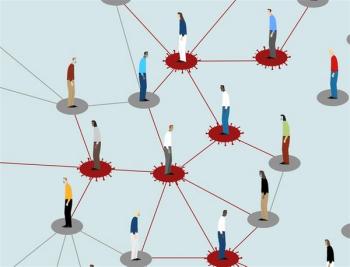
As the COVID-19 pandemic continues to surge, it is unlikely that contact tracing within healthcare will become anything less than critical.

Mary Ellen Beliveau: “If I’m an OB/GYN and all of a sudden I’m in the ICU, I don’t know how to run a ventilator. I’ve never run a ventilator before. I could be the best OB/GYN in the country. But suddenly, being put in a different area of practice and then to be expected to be at the top of my license is almost impossible.”

Investigators found SARS-CoV-2 "on various hospital objects, and these surfaces can be sources of nosocomial transmission via direct contact. Therefore, our findings provide an important basis for justification of strict contact precaution.”

Maya Gossman, RN: “I tell people, I put tubes in veins, that’s what I do for a living. Anytime you break the skin and you place a tube into the bloodstream, that’s a huge risk for infection.”