
Infection preventionists have the skill set to provide guidance beyond the health care setting. We know how to select PPE and how to use it. Cleaning and disinfection are like breathing to us.

Infection preventionists have the skill set to provide guidance beyond the health care setting. We know how to select PPE and how to use it. Cleaning and disinfection are like breathing to us.
If quick action isn’t taken, then the highly infectious B.1.1.7 variant of COVID-19 will become the main variant in the United States by March, further burdening our already overburdened health care system.
Infection preventionists need to educate primary health providers on the importance of utilizing monoclonal antibodies to prevent hospitalizations from severe COVID-19.

Linda Spaulding RN, BC, CIC, CHEC, CHOP: “There’s not enough literature out there yet to say that once you get the vaccine, you won’t get COVID again, and the literature that is out there says that once you get the vaccine, even if you don’t get COVID again, you can still be an asymptomatic carrier.”
It’s possible that infection preventionists and other health care workers who caught COVID-19 in the first wave can be reinfected.

Many members of environmental service teams feel underappreciated and these health care professionals are not trained in any systematic and continuous way, a study states.
Within the South African COVID strain scientists have found what they’re calling an “escape mutation” named E484K. It’s feared that this escape mutation will do just what the name implies—allow 501.V2 to escape vaccine antibodies.
Cedric Steiner: “But the nursing home…. One could make an argument that [infection control is] more important there in some ways, because you have those residents in smaller spaces."

Assume that everybody in a hospital setting is an asymptomatic carrier of COVID-19, two recent studies suggest.
The coming months will be telling in terms of how we approach quarantine and the implications of shortened quarantine periods. While it might be easier for people to adhere to, there is still concern for disease transmission.

For vaccines: Delivery doesn’t mean distribution. For variants: Their appearance underscores the importance of infection prevention methods.

Linda Spaulding RN, BC, CIC, CHEC, CHOP: “Infection preventionists need to learn how to clean an endoscope, or at least observe the cleaning…. Infection preventionists need to make rounds, they need to talk to the person processing.”

Kevin Kavanagh, MD: “One of the things that’s really frustrated me with this epidemic and pandemic is that people are totally focused on dying…. But in actuality, the disabilities are much, much more concerning because that is even affecting the young people.”
Yesterday, 3775 people died from COVID-19; that’s the highest single-day death total since the pandemic began, according to Johns Hopkins University. According to the COVID Tracking Project, 131,135 people were hospitalized yesterday for COVID-19, another single-day record.

The US and the world must appreciate the role of the pharmaceutical industry—the investigators, physicians and business leaders—who are rescuing the world from COVID-19. It’s the medical breakthrough of our lifetime.

Infection preventionists need to spread the message and articulate the uncertainties of this new variant of COVID-19. They need to emphasize that it is just not the old who are at risk and employ stricter containment measures.
Just how much more serious of a threat South Africa’s 501Y.V2 COVID variant represents has yet to be definitively answered, but British health officials argue that it’s much worse than the UK’s B117.

2021 will likely mean a mixture of things for infection preventionists (IPs). First, a focused effort on vaccine education. While this is a larger effort, IPs have always played a significant role in education and answering questions while rounding on the units and clinics.
Maureen Vowles: “I think that the relationship between infection preventionists and public health is key to the success of preventing CRAB and other multi-drug resistant organisms.”

Kristy Warren: “We need to do everything we can to help protect our providers when performing these aerosol generating procedures. And subsequently those providers that enter the room or exit the room after these procedures have occurred.”

Paula J. Olsiewski, PhD: “Healthcare workers at hospitals are always concerned about the air because historically, we know many disease agents are transmitted through the air, whether it’s measles or tuberculosis. Those appear on the scene long before COVID-19.”
Ravi Starzl, PhD: “If you’re constantly focused on trying to escalate the war of destruction, I think that the bacteria will always win that war. They just have too many countermeasures available to them and our rate of developing new antibiotics is far slower than their rate of developing countermeasures.”
Though tough months lie ahead for infection preventionists and other healthcare professionals, hope remains that at some point in 2021 things will begin to settle down. In the end, it comes down to a simple formula: We win, COVID-19 loses.

We must treat this strain with the respect it deserves, but we must not panic. There is no doubt that increased infectivity equates with increases in deaths, but it does not mean the vaccines will not work.

When it comes to COVID-19 vaccinations, it’s important to consider ancillary staff. Employees in environmental services, lab, respiratory therapy, physical therapy, and food services who have been working in high-risk areas.
Healthcare experts around the world worry that the COVID-19 mutation—called VUI–202012/01—might be 70% more infectious than the standard SARS-CoV-2 strain. There are no indications yet that it may also be more lethal or that vaccines can’t neutralize it.

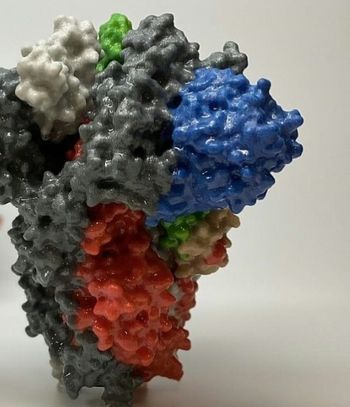
Unlike traditional forms, Moderna’s mRNA-1273 vaccine does not put weakened or inactivated germs inside the body. Rather, it teaches cells to make proteins that will trigger an immune response by injecting ribonucleic acid into cells which gives them instructions.

Officials at the Children’s Hospital of Philadelphia have the ability to convert several floors into airborne infection isolation rooms (AII), or more commonly termed negative pressure rooms, with the flip of a switch.

A panel of experts advising the FDA voted 20-1 (with 1 abstention) to tell the FDA that it should grant an emergency use authorization to Moderna's COVID-19 vaccine.

Bruce Y. Lee, MD, MBA: “We have to remember that infection control and prevention is not just dealing with the pathogen itself but dealing with the consequences and the downstream effects of what happens when you are dealing with the pathogen.”