
The CDC and FDA are expected to announce an immediate pause for administering the one-shot adenovirus Ad26.COV2.S while advising states distributing the product to consider doing the same.

The CDC and FDA are expected to announce an immediate pause for administering the one-shot adenovirus Ad26.COV2.S while advising states distributing the product to consider doing the same.

Those fully vaccinated had 90% protection against infection regardless of symptoms and even partial immunization yielded 80% protection against infection.

“APIC will be focused on conducting research on how health equity and health disparities should be addressed in the field of infection prevention and control including designing interventions…”

Infection preventionists (IPs) are now faced with delivering a difficult message. It is much easier to advocate for vaccinations which prevent disease, than it is for vaccinations which lessen the severity of disease or reduces your chances of becoming infected.

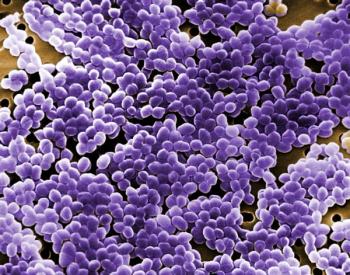
The study comes at a time when—despite all the attention and health care resources being thrown at COVID-19—medical experts have begun to turn a wary eye toward bacteriological pathogens.

When outbreaks have been reported in hospitals that are using universal masking, unmasked exposure to other health care workers is often the cause. Transmissions have been traced to break rooms and cafeterias.

The FDA wants providers to know about “contamination issues associated with reprocessing urological endoscopes, including cystoscopes, ureteroscopes and cystourethroscopes—devices used to view and access the urinary tract.”

Getting to know community pharmacists—in fact developing a professional rapport with those pharmacists—should be on an infection preventionist’s to-do list.

From a global health and infection prevention perspective, “normal” is what got us here—a state of poor preparedness, underfunded health departments, and neglected hospital preparedness for a pandemic.
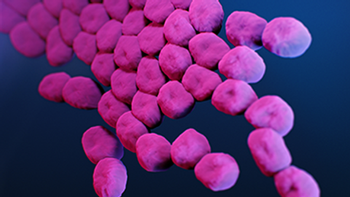
Priya Nori, MD: “The immediate thing that the health care industry has to grapple with, even as COVID hopefully starts to settle down after the mass vaccination campaign … [will be] superbugs.”

It is my advice that building managers seriously consider these measures, many of which are low cost and generate universal prevention measures.

“The COVID-19 pandemic has been a stark and painful reminder that nobody is safe until everyone is safe.”

The study states that it is “extremely unlikely” the pandemic virus occurred through a laboratory leak in Wuhan, China.

Evidence shows that bacteria on floors can be resuspended into the air with a potential of inhalation, swallowing, or contamination of surfaces and hands.


Here, we will review 3 common sterilization modalities currently in use for N95 respirator decontamination, how they work, and their strengths and limitations.

Infection prevention certification is not what it used to be—it is more valuable. It’s not for a few experts; it’s for the frontline IP in any health care setting that chooses to demonstrate competency.
Even assuming that up to 75% of people testing positive wouldn’t follow isolation guidance, the tests would greatly curtail infection, hospitalization, and death, argue investigators. The cost to the health care system would be worth it, investigators say.

Michael L. Millenson: “The CDC will pay more attention to infections. But there’s also an asterisk here. Will Congress continue to pay attention to infections? Will the administration’s budget continue to pay attention to infections? Will the media continue to pay attention to infections?”

Beau Wangtrakuldee, PhD: “In the health care industry in general, small sizes are typically based on Caucasian males, so once you get to women who truly have smaller frames there are no products available for them.”

The heavy burden on schools to reopen with distancing has increasingly become an issue as it often prevents fully reopening full classrooms, which is complex topic and one that carries with it a lot of nuance.

Arjun Srinivasan, MD: “There’s a lot of potential for synergy between the infection prevention program and the antibiotic stewardship program.”

Investigators propose that their simulation models can be used in educating nurses and other health care professionals about how best to maintain good hand hygiene, and also where best to put alcohol-based hand disinfectants.

The same mutation is found in the variant in Brazil but more disturbingly it is found in the New York variant.
No deadline was given for when these goals should be reached and some of the data to be used will depend on hospitals voluntarily releasing their numbers to the CDC.

Sharon Ward-Fore, MS, MT(ASCP), CIC: "We’ve learned the hard way that restaurants, office settings, hair salons, fitness centers, and schools have really suffered for the lack of guidance by professionals like infection preventionists."

SARS-CoV-2 is aerosolized. If a non-vaccinated person who is shedding the virus visits a vaccinated relative in a nursing home, he can easily spread the virus to all who reside in the facility.

That an entirely new outbreak of Ebola would be triggered by a latent infection 5 to 6 years after the initial infection is deeply worrisome.

COVID-19 outbreak hits Kentucky nursing home a week after CMS relaxes visiting restrictions.

The shape and material composition of the N95 respirators varied widely from manufacturer to manufacturer, which can result in variations in the efficacy of a particular method from one product to the next.