
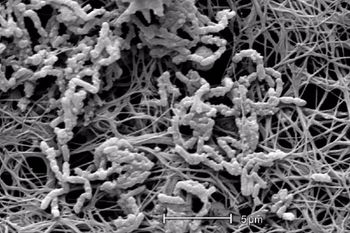
Maya Gossman, RN: “I tell people, I put tubes in veins, that’s what I do for a living. Anytime you break the skin and you place a tube into the bloodstream, that’s a huge risk for infection.”

Maya Gossman, RN: “I tell people, I put tubes in veins, that’s what I do for a living. Anytime you break the skin and you place a tube into the bloodstream, that’s a huge risk for infection.”

Nancy Moureau: “Our priority is to minimize infections or potentially even to eliminate them. We want complications to be history. In order to achieve those goals, I see the vascular access specialist or the vascular access teams as being in a partnership with the infection preventionist.”

The discussion and research underscore the potential advantages of vascular access services teams (VASTs) for assessment, insertion, management, complications reduction, and staff education.
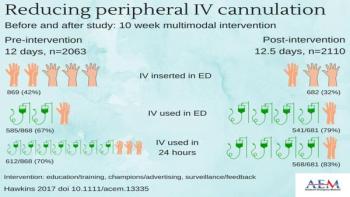
The mixed-method, prospective, observational before-after study was performed in a large tertiary academic children’s hospital in the Netherlands and included a preintervention period and an intervention period.













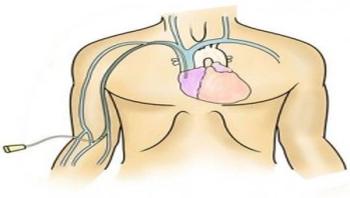





It has been more than 10 years since The New England Journal of Medicine published the Keystone project’s ground breaking work on reducing ICU CLABSIs using a central line insertion bundle. Since that time, this has become the absolute standard throughout healthcare settings in the United States. When it comes to completing the central line insertions checklist, many of us only accept “yes” and “yes with prompting” as possible responses. Our accrediting agencies expect this as a standard of practice.
