COVID-19
Latest News
CME Content

We are forced to act on best evidence, but in some cases the evidence is less than actionable.

Lisa Brosseau, ScD: "What we’re seeing is a lot of magical thinking. A lot of wishful thinking. Cloth masks are wishful thinking."

Nicole York: "The dying process can take a long time, but I was with her while she was still alert. And I called up her family so that they could talk to her on the phone. But that’s all she got was just to talk to them on the phone."

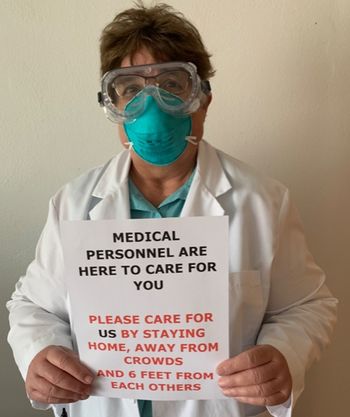
Look to our own practices in hospitals. Are meetings occurring with lots of people for a prolonged period of time without PPE? Breakroom clusters of staff to eat? Exposure is not limited to the patient-caregiver interaction.

Kalia Murray, EMT: "We are the first ones to arrive on a scene, often having no idea what we're walking into."

As we emerge from the COVID-19 crisis, it’s very important for infection control professionals to think, “How do we take this crisis and use it as a lever to cause the change that we care about so much?”

Deborah Birx, MD, the Coronavirus Response Coordinator: “Throughout the summer, when we do not have flu to contaminate the picture, we’ll be able to follow the syndromic pattern city by city, community by community, state by state."

The CDC’s recommendation of using a bandana as a last resort to stop the COVID-19 virus places our healthcare system at the level of a third-world country and underscores the severity of the current pandemic and erosion of our healthcare system’s infrastructure.
"We have to be comfortable with the fact that we have to reuse PPE for multiple patients. But one of the things they have to remember is those multiple patients all have the same illness. So, it’s not like we’re going to transfer multi-drug resistant organism to the next patient. Because we try not to use the same PPE for those situations."

Healthcare workers often have the foresight to know when patients are positive, while knowledge of cases in the community is less likely.

There are nearly 10,000 STERRAD Sterilization machines in about 6,300 US hospitals, and the reprocessing times vary from 55 minutes, to 28 minutes, and 24 minutes, depending on which particular STERRAD machine is being used.

At a hospital that recently announced layoffs during the COVID-19 crisis, hospital executives agreed to a 20% pay cut. That sounds impressive but the CEO makes over $1.9 million a year and the corporation has net assets or fund balances of $1.6 billion. Meanwhile, the shortage of N95 face masks for healthcare workers continues.

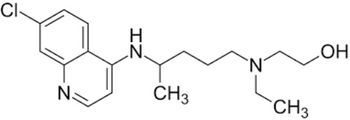
If you are on one of these medications one should perform strict social distancing and protect yourself from contracting COVID-19.

Harvey V. Fineberg, MD, PhD: “If we take these six steps to mobilize and organize the nation, we can defeat COVID-19 by early June.”

As an infection preventionist, I found these to be helpful in establishing plans, training methods, and more.

In Washington State, a choir practice of 60 individuals who practiced social distancing resulted in 45 infections, 3 hospitalizations and 2 deaths.


N95 masks are in high demand but so are surgical masks, isolation gowns, thermometers and disinfecting wipes.

According to the United States Conference of Mayors, cities need 28.5 million face masks, 24.4 million other pieces of PPE equipment, 7.9 million COVID-19 test kits, and 139,000 ventilators.
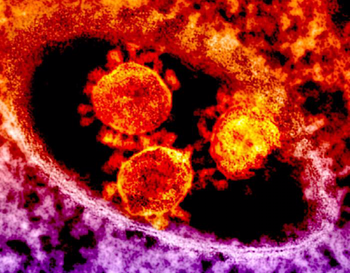
ACE inhibitors up regulate (increase) the ACE2 receptor. This is the receptor the COVID-19 virus uses to attack the lungs.
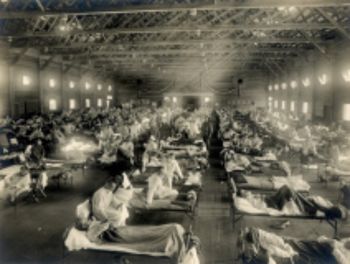
The Spanish flu of 1918 killed between 20 and 50 million people. What lessons can we take from it?