
Linda Spaulding RN, BC, CIC, CHEC, CHOP: “Infection preventionists need to learn how to clean an endoscope, or at least observe the cleaning…. Infection preventionists need to make rounds, they need to talk to the person processing.”

Linda Spaulding RN, BC, CIC, CHEC, CHOP: “Infection preventionists need to learn how to clean an endoscope, or at least observe the cleaning…. Infection preventionists need to make rounds, they need to talk to the person processing.”
Maureen Vowles: “I think that the relationship between infection preventionists and public health is key to the success of preventing CRAB and other multi-drug resistant organisms.”
Though tough months lie ahead for infection preventionists and other healthcare professionals, hope remains that at some point in 2021 things will begin to settle down. In the end, it comes down to a simple formula: We win, COVID-19 loses.

Infection preventionists can work with environmental services (EVS) leadership to implement a routine practice for quality assurance checks that EVS leadership can follow. These metrics can then be reviewed as an aggregate with the IP department to target whether further education may be beneficial.
At this point, since 2014, we all have improved our ability to respond to and prevent emerging infectious diseases, so why not make this practice a permanent part of infection control and not just one that comes up ad hoc?
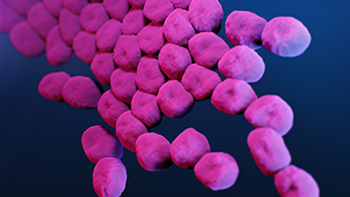
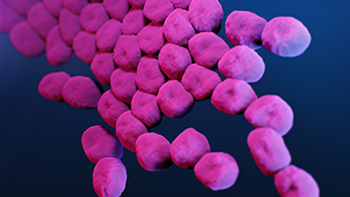
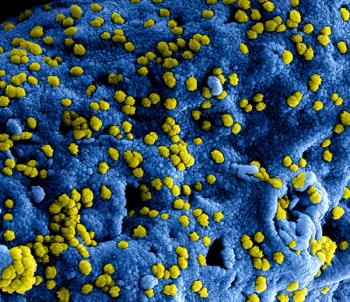
When an 850-bed urban hospital fought off COVID-19 in part by having to relax infection prevention protocols, the opportunistic and deadly carbapenem-resistant Acinetobacter baumannii (CRAB) struck.
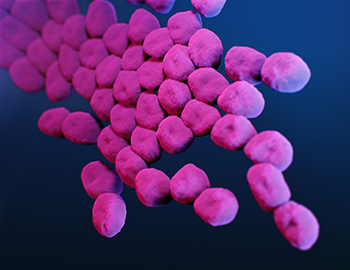
CRAB has chameleon-like tendencies that allow it to absorb material from other organisms, and that allows it to ward off most antibiotics. It’s a Superbug.
Study: “These results strongly recommend routine daily cleaning of mobile phones for effective reduction of device contamination; moreover, medical staff should perform hand hygiene before and after using mobile phones.”

During the period that employees wore a monitoring badge, compliance with hand hygiene protocols increased significantly.

Danish investigators wanted to see if a nudge provided by a green smiley face light on dispensers of alcohol-based disinfectant would improve hand hygiene compliance of nurses and doctors. It did. Greatly.

Michael Millenson: “When you dig a little deeper, you end up though with some questions. We’re a big country, and this is an enormous crisis. Well, $180 million? You can barely buy a couple of US senators with that.”

If you are an infection preventionist and are not currently involved in product review, now may be a great time to reach out to your supply chain team to explain the perspective you can bring to the table and ask to be involved.
New infection preventionists can use this checklist to perform IP rounds in the surgical suite, decontamination areas, and sterile processing area.

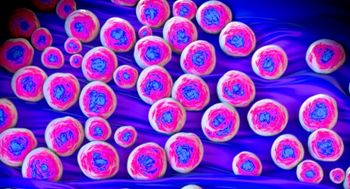
Candida auris is difficult to identify with standard laboratory methods. It can be misidentified in labs without specific technology, which can lead to mismanagement.

The odds of a viral outbreak such as SARS-CoV-2 in custodial settings, such as prisons and juvenile detention centers, are high. But video surveillance already in place in the facilities can enhance contact tracing.

Michael Bell, MD: “The challenge that infection control professionals face has grown tremendously. We’re asking these individuals to not only be experts, but also to take responsibility for such a wide range of activities ... and finding ways to help them accomplish what they’re doing across the whole population of healthcare personnel is the rationale behind Project Firstline.”

Discussions about hospitalizations should include those of healthcare personnel who have been hospitalized with COVID-19. This is something that has been a gap in our data but increasingly discussed.
Too many hospitals apparently do not use the CDC’s Hospital Toolkit for Adult Sepsis Surveillance, which may explain the number of healthcare-acquired infections that remain unreported.

When healthcare workers using the red box stepped into the patients’ rooms, there was “significantly increased non-compliance” with PPE and hand hygiene protocols compared to those healthcare workers who went into rooms without red boxes.

Investigators found that the mean healthcare cost for treating elderly influenza patients per patient per flu season ranged from $3,299 to $12,398 higher than the costs for treating patients with congestive heart failure, chronic obstructive pulmonary disease, coronary artery disease, and stage 5 renal disease.

Investigators found that a prompt on a disinfection tracking system led to an increase rate of the disinfection of computers on wheels at a veterans’ hospital in Texas.

CAUTI rates were 83% higher and CLABSI rates were 65% higher in the COVID-19 units compared to the non-COVID-19 units.

There are 4 “moments” involved as a healthcare professional at a long-term care facility (LTCF) weighs whether to prescribe an antibiotic to a patient or resident.

When COVID-19 struck, the proper use of PPE and greater attention to hand hygiene and cleaning surfaces became the norm. When that happened, rates of Clostridium difficile decreased significantly.
Sarah Smathers, MPH, CIC, FAPIC: “I think that hospital administrators are concerned about how they’re going to recruit in a field that is expecting a lot of retirees: 40% of infection professionists are expected to retire in the next five to 10 years.”