
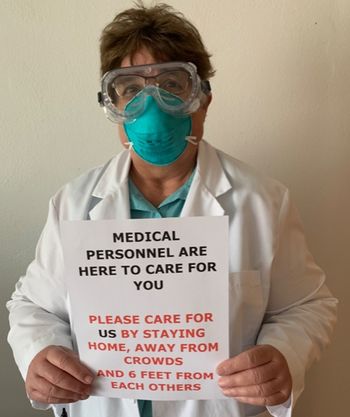
Especially in healthcare settings, when infection preventionists need to explain protocols and guidelines to their fellow healthcare workers and patients, something can always be lost in translation if much of the face remains hidden.


Especially in healthcare settings, when infection preventionists need to explain protocols and guidelines to their fellow healthcare workers and patients, something can always be lost in translation if much of the face remains hidden.

Linda Spaulding: “We [infection preventionists] have listening sessions with staff and we talked to them about proper mask wearing 24/7. We can do a listening session and we still have people sitting there with a mask under their nose, while we’re telling them not to. You have to continuously stress this among healthcare workers, be it whatever department.”

Neck gaiters weren’t the only face coverings tested: in all 14 were analyzed, from N95s (unsurprisingly judged to be the most effective in containing COVID-19 spread) to bandanas (not much more effective then neck gaiters, according to the study).

Film healthcare workers as they don and doff N95s, show that video to participants (explaining where they got it right, and where they got it wrong), and then have the participants don and doff again with more input from trainers.

Many factors make the isolation precautions for diseases like COVID-19 more complex than typical droplet or airborne definitions.

Maureen Spencer, RN, M.Ed.: “The World Health Organization did come out and said that they support the concept that this is droplet and airborne. And what that does is it changes our approach for infection prevention.”

It will also be necessary to again train other professionals the way IPs have historically trained them about infection prevention, because a lot of the old rules had to be set aside when COVID-19 surged.
We have much work to do in terms of risk communication and awareness. This is a good example of how quickly exposures can happen in the workplace when we focus only on employee-to-customer interactions or healthcare worker-to-patient interactions.
The filtering face piece respirators will be manufactured at General Motor’s facility in Warren, Mich. The company had to revamp its manufacturing process to accommodate making the respirators, creating four separate assemble stations.

Harry Peled, MD: “I think for administrators and infection control people, the attitude has to be there is enough evidence that the wearing of N95s should be official. The claim that we’re going to wait for perfect evidence is just not tenable. We don’t do that for anything else in medicine.”

Investigators argue in the Annals of Internal Medicine that all healthcare workers in inpatient settings caring for COVID-19 patients should be equipped with N95s.

Healthcare workers are particularly susceptible to maskne because they tend to wear their masks for extended periods.

N95 decontamination must meet 3 criteria. It needs to: inactivate the pathogen, it can’t damage or degrade the N95 in any way, and it should not introduce an additional hazard to the healthcare worker.

Just-in-time (JIT) fit testing allows a healthcare organization to offer evaluation, training, and fitting of HCPs during rapid intervals, as needed, based on specific patient care assignments.

Decontaminated respirators should only be resorted to when unused devices are not available, but that happened a lot in the last few months.

The wearing of cloth masks doesn’t mean that employees should stop following social distancing guidelines. In fact, social distancing guidelines must be followed at all times.

Viral droplets from a sneeze can even travel 23 to 27 feet.

One hospital has asked workers to consider shaving their beards.

Face shields are durable and can be cleaned and reused repeatedly, thereby eliminating the problem of shortages.

Because of the shortage of N95 masks, surgical masks have been used. But they don't offer nearly the same protection.

Lisa Brosseau, ScD: "What we’re seeing is a lot of magical thinking. A lot of wishful thinking. Cloth masks are wishful thinking."

Lives are at stake and counterfeit N95 respirators make things worse for infection preventionists and others trying to care for COVID-19 patients. If you suspect that something being billed as an N95 is fake, report it to the CDC.

National Nurses United and the California Nurses Association, declared victory because hospital administrators “announced that health care workers throughout the Providence system will be issued N95 respirator masks to wear when caring for COVID positive or potentially COVID positive patients…,” according to a press release issued by the unions.
"We have to be comfortable with the fact that we have to reuse PPE for multiple patients. But one of the things they have to remember is those multiple patients all have the same illness. So, it’s not like we’re going to transfer multi-drug resistant organism to the next patient. Because we try not to use the same PPE for those situations."
