Even with effective screening, treatment, and education, STIs can be like movie villains who just won’t die, who change form, and who keep coming back to wreak havoc. They’re relentless, but so is science.
Even with effective screening, treatment, and education, STIs can be like movie villains who just won’t die, who change form, and who keep coming back to wreak havoc. They’re relentless, but so is science.

Linda S. Estep, BS MT (ASCP), CIC: “I’ve done many hand hygiene audits in my day, I still do hand hygiene audits, when I’m in the hospitals now. If they know who you are, they scatter. They know the infection preventionists.”

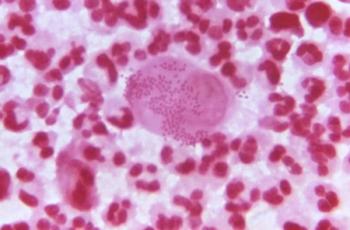
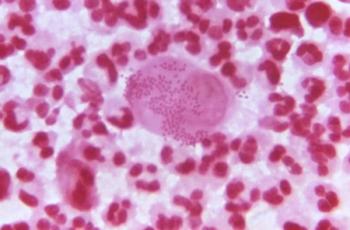
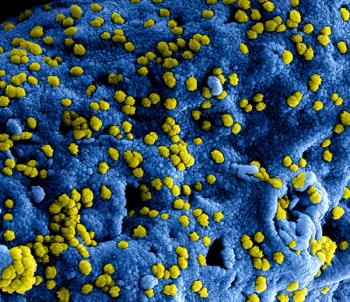
Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.
Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.

Hand hygiene is always important, but during this pandemic it’s crucial to preventing transmission. Now technology is making it possible for hospitals not only to monitor compliance, but also potential viral exposure.
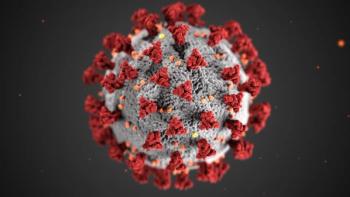
Though tough months lie ahead for infection preventionists and other healthcare professionals, hope remains that at some point in 2021 things will begin to settle down. In the end, it comes down to a simple formula: We win, COVID-19 loses.
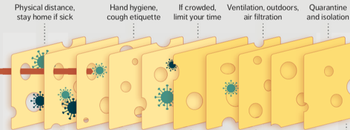
In essence, infection prevention and control isn’t just one measure, like personal protective equipment (PPE), but all of these layers. Each layer is imperfect but plays a critical role in reducing risk.
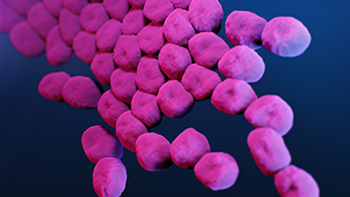
When an 850-bed urban hospital fought off COVID-19 in part by having to relax infection prevention protocols, the opportunistic and deadly carbapenem-resistant Acinetobacter baumannii (CRAB) struck.
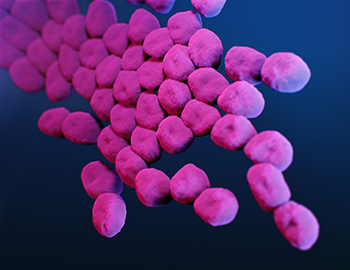
CRAB has chameleon-like tendencies that allow it to absorb material from other organisms, and that allows it to ward off most antibiotics. It’s a Superbug.
Study: “These results strongly recommend routine daily cleaning of mobile phones for effective reduction of device contamination; moreover, medical staff should perform hand hygiene before and after using mobile phones.”

During the period that employees wore a monitoring badge, compliance with hand hygiene protocols increased significantly.

Danish investigators wanted to see if a nudge provided by a green smiley face light on dispensers of alcohol-based disinfectant would improve hand hygiene compliance of nurses and doctors. It did. Greatly.
New infection preventionists can use this checklist to perform IP rounds in the surgical suite, decontamination areas, and sterile processing area.

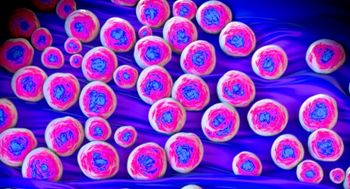
Candida auris is difficult to identify with standard laboratory methods. It can be misidentified in labs without specific technology, which can lead to mismanagement.

The investigators say that their findings underscore the importance of encouraging and “empowering” patients to be a part of efforts to improve hand hygiene compliance among healthcare workers.

Michael Bell, MD: “The challenge that infection control professionals face has grown tremendously. We’re asking these individuals to not only be experts, but also to take responsibility for such a wide range of activities ... and finding ways to help them accomplish what they’re doing across the whole population of healthcare personnel is the rationale behind Project Firstline.”
Too many hospitals apparently do not use the CDC’s Hospital Toolkit for Adult Sepsis Surveillance, which may explain the number of healthcare-acquired infections that remain unreported.

When healthcare workers using the red box stepped into the patients’ rooms, there was “significantly increased non-compliance” with PPE and hand hygiene protocols compared to those healthcare workers who went into rooms without red boxes.

Investigators found that the mean healthcare cost for treating elderly influenza patients per patient per flu season ranged from $3,299 to $12,398 higher than the costs for treating patients with congestive heart failure, chronic obstructive pulmonary disease, coronary artery disease, and stage 5 renal disease.

Investigators found that a prompt on a disinfection tracking system led to an increase rate of the disinfection of computers on wheels at a veterans’ hospital in Texas.

CAUTI rates were 83% higher and CLABSI rates were 65% higher in the COVID-19 units compared to the non-COVID-19 units.

There are 4 “moments” involved as a healthcare professional at a long-term care facility (LTCF) weighs whether to prescribe an antibiotic to a patient or resident.
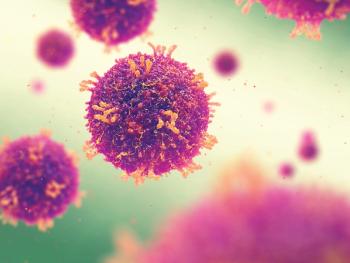
Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.

When COVID-19 struck, the proper use of PPE and greater attention to hand hygiene and cleaning surfaces became the norm. When that happened, rates of Clostridium difficile decreased significantly.

Bug of the Month helps educate readers about existing and emerging pathogens of clinical importance in healthcare facilities today.