News



A new, computer-based screening method could reveal the virus-fighting potential of drugs originally developed to treat other conditions, reports a study in PLOS Computational Biology.

Mosquito saliva influences transmission of viruses to a bitten mammalian host. For example, it contains factors that dampen the host immune response and so facilitate infection. A study published in PLOS NTDs reports on a saliva protein with the opposite effect: D7, a protein present in Aedes aegypti saliva, binds to Dengue virus (DENV) and inhibits its transmission to human cells and mice. Antibodies against D7, which are present in humans exposed to mosquito bites, might therefore facilitate virus transmission and enhance disease severity.









The Standard Precautions concept in healthcare dictates that healthcare workers assess risk in advance of a patient interaction and use appropriate interventions such as barriers, hand hygiene, and/or surface disinfection, to address the risk and prevent becoming contaminated by the patient or the patient’s environment. This approach has generally been credited with helping hospital employees protect themselves from acquiring infectious agents on a daily basis. However, a growing body of research has called into question whether this approach is in fact adequate.







The medical field has known for almost 200 years that disinfecting hands saves lives by reducing the ability to carry disease. But even in 2016, global hand hygiene compliance remains shockingly low. At any given time, the World Health Organization (WHO) notes the presence of at least 1.4 million healthcare-associated infections (HAIs), even as the nonprofit accreditation body the Joint Commission has dubbed hand hygiene “the most important intervention for preventing HAIs.”


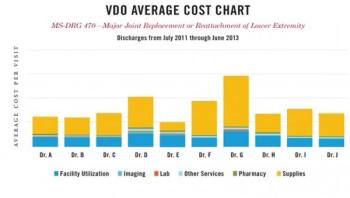
Bucking national trends, a new study shows that a program is making a difference in healthcare quality and cost. Developed by University of Utah Health Care (UUHC), the so-called value driven outcomes (VDO) program breaks down health procedure costs to the level of each bandage and minutes of nursing time, revealing variability that is otherwise hidden from view. After addressing inefficiencies exposed in three common procedures -- joint replacement, in-hospital laboratory testing, and sepsis management – patients fared better and costs fell by up to 11 percent. The results were published online in the Journal of the American Medical Association (JAMA) on Sept. 13.