
Videos
Latest News
Latest Videos

CME Content
More News

The HSPA 2022 presentation focused on sharing new and future sterilization standards updates.

Jill Holdsworth, CIC, FAPIC, NREMT, CRCST, manager of infection prevention at Emory University Hospital Midtown, joins ICT® to discuss the implications of her research, as well as other guidance for building an optimal relationship between infection prevention and the sterile processing department.

Previously, reduction of other organisms, like VRE, C difficile, and MRSA had been demonstrated by this combination.

Remembering the COVID-19 pandemic and supply chain issues, investigators study the efficacy of reusing N95 FFRs.

Susan “Suzy” Scott, MSN, RN, WOC Nurse, also speaks to Infection Control Today® about incident tracking and electronic medical records.

After an Expo like no other, Dennis looks forward to the 70th year of advocacy for perioperative nurses.

A recent study's results also could indicate how other vaccinations, including COVID-19 and pneumonia, affect patients.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 25.

Investigators concluded that HCPs can safely return to work after 7 days of quarantine if they test negative for COVID-19 on days 5 to 7.

The system gives infection preventionists another tool to combat the pathogen despite implementation challenges.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending March 11.

Key recommendations in the report include normalizing mask wearing and avoiding the supply chain failures.
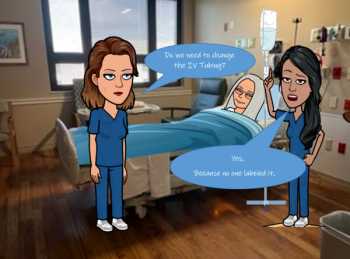
Compliance has increased up to 50% on key infection prevention and control practices at a South Carolina health system due to these short emoji-cartoons.
Staff shortages, public recognition, and moving out of the medical field are all issues that the sterile processing industry has faced.

Lisa Waldowski, DNP, RN, CIC, of Kaiser Permanente: “There will always be a role for infection preventionists. I don’t worry about job security, so to speak. There are so many elements within infection prevention and control.”

Jamie Seltzer: “We have so much history—recent history as well as 100 years ago—to tell us that it would be incredibly unusual and atypical if SARS-CoV-2 were the only viral infection that did not lead to post-viral complications.”

Proper ventilation can greatly reduce the environmental strain on operating rooms. However, there’s no one-size-fits all solution.

Just when should a health care professional return to work after a high-risk COVID-19 exposure? In a Q&A, Sharon Ward-Fore, MS, MT(ASCP), CIC, FAPIC, explains the CDC’s changing recommendations.
Anthony Harris, MD, MBA, MPH: “There are nights where I go to bed thinking, ‘Will tomorrow be the day that I read about a tremendous increase in severity in Omicron, and antibody dependent enhancement could be the cause of it?’”

CDC’s Michael Craig: “Every country is an importer and an exporter of resistance…. And our hope is that this could be a jumpstart to help some of these countries start to build the capacity that is needed everywhere.”

La’Titia Houston MPH, BSN, RN, CIC: “We work not only with the bedside nurses and the sterile processors, but even with our clinicians, our physicians. They want a timeout before the procedure is even performed because they want to ensure that the scope did pass during the high-level disinfection procedure.”

Kevin Kavanagh, MD: “The deer apparently live with COVID-19 quite well, but, yet rapidly spread it amongst the herds. And that’s actually very problematic, because if it finds a host that it doesn’t make sick, but yet it can mutate and change and then reinfect other animals and plus mankind, that is one of the worrisome scenarios that could take place.”

One of many presentations at the ISSA Show North America 2021 this week seeks to light an entrepreneurial fire under an old concept.

Crystal Heishman, MBA, MSN, RN, ONC, CIC: “You don’t ever want to go into a sterilization department and say, ‘You’re doing this wrong’. Because they’re the subject matter experts. You want to learn. You want to learn the process. You want to work together because it makes a stronger partnership.”

Doe Kley, RN, CIC, MPH,T-CHEST: “We just can’t keep doing what we’ve been doing with our singular focus on one pathogen. We know that while we were doing that—while we were so busy with COVID-19—other really dangerous and emerging pathogens got a foothold. The one that scares me the most is Candida auris.”














