
U.S. Trade Representative Katherine Tai: “The administration believes strongly in intellectual property protections, but in service of ending this pandemic, supports the waiver of those protections for COVID-19 vaccines.”

Saskia v. Popescu, PhD, MPH, MA, CIC is an infection preventionist and infectious disease epidemiologist. Currently, she serves as a senior fellow at the Council on Strategic Risks, where she works to address global health security issues, including national policies impacting health care readiness and biodefense. Saskia is also an assistant professor at George Mason University, teaching courses on health care preparedness and epidemiology in policy. She holds a PhD in biodefense from George Mason University, where her research focused on the political and economic obstacles to investing in infection prevention, a MPH in infectious disease epidemiology, a MA in international security studies--both from the University of Arizona. Prior to her work at CSR, Saskia helped lead global health response at Netflix and was a senior infection preventionist with HonorHealth in Arizona. She has worked with the WHO, supported multiple NASEM workshops and reports, and supports NGO engagement within the Biological Weapons Convention at the UN. Saskia’s work is on building health care biopreparedness and readiness for infectious disease threats, especially in larger global health security efforts.

U.S. Trade Representative Katherine Tai: “The administration believes strongly in intellectual property protections, but in service of ending this pandemic, supports the waiver of those protections for COVID-19 vaccines.”

During this time, as hospital case counts drop, IPs are expected to just switch back to normal while still ensuring a readiness to respond to COVID-19.

The truth is that variants will occur where the virus spreads and until SARS-CoV-2 is controlled everywhere, it won’t be controlled anywhere. What is occurring in India is a prime example of this.

It’s important to match COVID-19 masking rules to reasoning behind them.

The number of syphilis cases in 2000 raised hopes that it could be eradicated, but since 2015 cases have risen 74%.

Those fully vaccinated had 90% protection against infection regardless of symptoms and even partial immunization yielded 80% protection against infection.

From a global health and infection prevention perspective, “normal” is what got us here—a state of poor preparedness, underfunded health departments, and neglected hospital preparedness for a pandemic.

The heavy burden on schools to reopen with distancing has increasingly become an issue as it often prevents fully reopening full classrooms, which is complex topic and one that carries with it a lot of nuance.

That an entirely new outbreak of Ebola would be triggered by a latent infection 5 to 6 years after the initial infection is deeply worrisome.

Yes, fully vaccinated people can relax some of the social distancing protocols that we’ve all been chaffing under this year. However, understand the nuances.

Infection prevention isn’t unique to health care, but rather representative of a bigger role within the community – it’s where health care and public health meet.

As more people become vaccinated, we will be navigating the aspects of a partially vaccinated public. This will be especially challenging as we learn more about prevention of infection and not just severe disease.

As all resources and attention were focused on COVID-19 for the past year, many other infectious diseases were neglected. Here’s what we need to monitor.

Double-masking can prove more cumbersome for many. If the goal is to protect the mask underneath, perhaps consider a face shield or a strategy for cleaning the mask more frequently.

Contact tracing is reactive—the goal is to avoid these close contact exposures in which people are interacting without masks and indoors. Practice makes permanence after all.

The topic of in-person school has been a heated one as the epidemiology around children has been something that’s taken a while to understand.
There are pieces of novel variants that we’re still learning about, like the impact to therapies and how these variants might affect what we know about COVID-19, like reinfection.
The coming months will be telling in terms of how we approach quarantine and the implications of shortened quarantine periods. While it might be easier for people to adhere to, there is still concern for disease transmission.

For vaccines: Delivery doesn’t mean distribution. For variants: Their appearance underscores the importance of infection prevention methods.

2021 will likely mean a mixture of things for infection preventionists (IPs). First, a focused effort on vaccine education. While this is a larger effort, IPs have always played a significant role in education and answering questions while rounding on the units and clinics.

When it comes to COVID-19 vaccinations, it’s important to consider ancillary staff. Employees in environmental services, lab, respiratory therapy, physical therapy, and food services who have been working in high-risk areas.
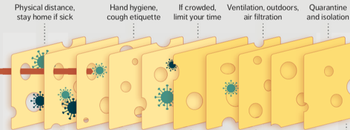
In essence, infection prevention and control isn’t just one measure, like personal protective equipment (PPE), but all of these layers. Each layer is imperfect but plays a critical role in reducing risk.
At this point, since 2014, we all have improved our ability to respond to and prevent emerging infectious diseases, so why not make this practice a permanent part of infection control and not just one that comes up ad hoc?

Strategies are needed to reduce the risk of COVID transmission between the breastfeeding mother and newborn. Meanwhile, mask mandates work.

The CDC may lower the days someone needs to be quarantined because of COVID exposure from the current 14, to from 7 to 10 days. That range is troublesome: Which is it, 7 or 10?

IPs have not only that frontline experience, but also the ability to pivot and evolve with recommendations. In fact, our very jobs are about translating continuously evolving evidence and guidance into practice.

Healthcare workers are vigilant about personal protective equipment (PPE), hand hygiene, and disinfection efforts in the hospital when managing COVID-19 patients. Too often, though, they let their guard down when they get home.

Discussions about hospitalizations should include those of healthcare personnel who have been hospitalized with COVID-19. This is something that has been a gap in our data but increasingly discussed.

It’s no longer just a matter of case counts and hospitalizations due to COVID-19, but it’s what we’re seeing in terms of the demographic groups being affected and associative complications.

It can be helpful for infection preventionists to still provide quick COVID-19 rounds in units and high-risk areas like emergency departments and urgent care clinics. These can be as simple as 30-minute reviews of personal protective equipment, isolation precautions, and communication pathways.