
A hospital system in India was able to vaccinate 90% of health care workers in part by using role models, photos, and social media, according to a new study.

A hospital system in India was able to vaccinate 90% of health care workers in part by using role models, photos, and social media, according to a new study.

No health care worker is immune from the dangers of handling sharps. Physicians hold a rate just under that of nurses, mostly related to use of scalpels, but are less likely to report these injuries.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending November 12.

What does the post-COVID-19 future look like for infection preventonists? Great strides in infection prevention have been made because of the COVID-19 response, but look for them to be modified moving forward.

Adenosine triphosphate (ATP) bioluminescence needs technological enhancement if it’s to reach its full potential as a disinfection tool, says a study.

No agreed-upon definition exists that spells out exactly which symptoms trigger the need for a test. One expert says that if a get-together includes, for example, someone with Stage 4 cancer, it would be appropriate for all attendees to test beforehand.

All signs point to finally throwing off the dictatorship of the little spiky ball.

The availability of pediatric vaccines is being presented as a way to return to some sense of normal after two years of a pandemic.

Crystal Heishman, MBA, MSN, RN, ONC, CIC: “You don’t ever want to go into a sterilization department and say, ‘You’re doing this wrong’. Because they’re the subject matter experts. You want to learn. You want to learn the process. You want to work together because it makes a stronger partnership.”

Doe Kley, RN, CIC, MPH,T-CHEST: “We just can’t keep doing what we’ve been doing with our singular focus on one pathogen. We know that while we were doing that—while we were so busy with COVID-19—other really dangerous and emerging pathogens got a foothold. The one that scares me the most is Candida auris.”
Many believe that super immunity can develop in those who have had SARS-CoV-2 infections and have become vaccinated. Meanwhile, fully vaccinated might mean getting 3 doses, not 2.

Darrel Hicks: “EVS teams work around professionals who are certified—whether it’s respiratory therapists, physical therapists, the RNs, the doctors—and I think if we ever hoped to elevate their status that we need to certify environmental services workers to a certain level of knowledge before they even start cleaning patient rooms.”
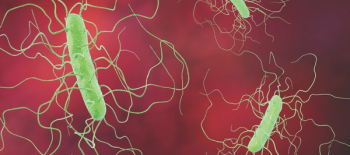
The use of almost every antibiotic increases the chances of Clostridioides difficile infection, and that includes the drugs that are used to treat C diff, a study states.
In order of occurrence, the most common types of HAIs are catheter-associated urinary tract infection (CAUTI) at 32%; surgical site infection (SSI) at 22%; pneumonia (ventilator-associated pneumonia) at 15%; and central-line associated bloodstream infection (CLABSI) at 14%.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending October 29.

Vetting new technology and products is a complicated endeavor that takes hours if not weeks before a decision can be made as to whether to bring products into a health care facility. The COVID-19 pandemic did not give health care the luxury of time.
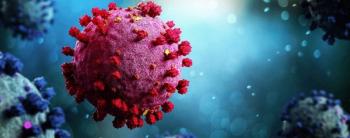
As of today, the outlook is very good and the pandemic is on a trajectory of burning out, but there are valid concerns which require that we continue our vigilance and public health strategies.

One of the most disturbing features of C auris is that, in its relatively short life, it has rapidly developed resistance to the few available treatment options.

Infection preventionists have been measuring hand hygiene with very little change in practice or retention of proper practice. Now is the time to think of new ways to improve hand hygiene and patient outcomes.

The move is the first step in paving the way for younger children to get COVID-19 vaccines.

Compared to cases confirmed by human clinical testing, the air sampling used in the college dorms in the study had a success rate of 75%–100% in detecting infection by SARS-CoV-2.

The term “mild COVID-19” is an oxymoron. The devastating long-term effects of long COVID, along with future emergence of cardiovascular disease in those with minimal initial symptoms, reminds us that all SARS-CoV-2 infections may pose grave dangers to those who contract the virus.

Moderna’s phase 2/3 pediatric trial showed a lesser dose of the company’s 2-dose COVID-19 vaccine mRNA-1273 is associated with a significant neutralizing antibody response in children aged 6 to <12 years old.

Jason Tetro, author of The Germ Code: “Moving forward, I think we’re going to be going into this idea of seasonality, or as I like to say, cold, flu and COVID-19 seasons.” And the so-called "monster variant"? It's already here, says Tetro. It's called Delta.

Take 5 minutes to catch up on Infection Control Today’s highlights for the week ending October 22.