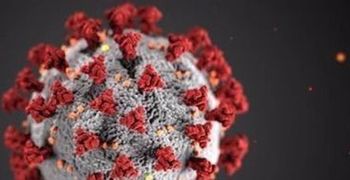
Some medical experts say that in this case, inaction is also an action—either the US gives boosters or does not. That decision needs to be based on the best available evidence. Instead, there seems to be a desire to wait another 6 months for pristine randomized controlled studies.