
Tori Whitacre Martonicz

Tori Whitacre Martonicz, MA, is the lead editor of Infection Control Today. She has been a writer and editor for over 30 years and has an MA and BA in English Composition/Literature from the University of Akron in Akron, OH. She lives in Ohio with her husband, Eric; son, Drake; 2 tiny dogs, Selena Brigid Sophia and Doctor Danger Dog; and a big black cat, Freya. She loves reading, writing, gardening, and spending time with her loved ones.
Contact her through her email: tmartonicz@mjhlifesciences.com.
Articles by Tori Whitacre Martonicz



As hospitals seek stronger defenses against health care-associated infections, experts are turning their attention to an unexpected source: copper-infused linens. Learn how, supported by emerging science and real-world feasibility, these textiles may offer a practical and effective way to lower microbial loads and enhance infection prevention bundles in this installment of a recent roundtable on linen issues.

HSPA President Arlene Bush believes the sterile processing profession is stronger—and more essential—than ever. From expanding public awareness to evolving standards and global reach, Bush says the field is driven by dedicated professionals who “do amazing things, 365 days a year,” and deserve recognition for their expertise, resilience, and impact on patient safety.

As hospitals search for new ways to reduce environmental bioburden, copper-embedded textiles are emerging as a promising tool. In this second installment of ICT's recent panel discussion, experts described how these soft, everyday fabrics can rapidly kill microbes, sustain their effectiveness between washes, and strengthen infection control bundles across care settings.

From hospital beds to privacy curtains, textiles may be one of the most underestimated contributors to health care-associated infections, according to experts who say these everyday items deserve far more attention in prevention bundles.

Hand, foot, and mouth disease is spiking across parts of the US, with some states reporting record numbers of outbreaks. Experts say environmental conditions, shifting immunity, and new viral strains may be driving this year’s rapid rise.

Missed opportunities, Graves warned, place patients at risk. Many surgical patients are immunocompromised, and a stethoscope may come near the incision. “Regardless of the scenario, [cleaning the stethoscope] each time is going to protect patients.”

Stethoscope hygiene, UV technology, and dwell time failures took center stage in this second installment of a panel of experts explored why routine disinfection still lags and what must change in clinical practice.

At IDWeek, Mohammad Enayet Hossain, PhD, from ICDDR,B, shared a breakthrough: a portable point-of-care test that works in half an hour and has strong accuracy against RT-PCR. A huge step forward for outbreak readiness.

In this provocative interview, Kevin Outterson, JD, LLM, explains why infection prevention benefits society but costs hospitals, urging fire department–style funding and PASTEUR incentives that reward diagnostics, stewardship, and antibiotic use.

Much is discussed about stethoscopes, the "third arm" of clinicians, but what about the risk of spreading health care-associated infections?

Two unsettling zoonotic developments are testing the limits of infection prevention and public health vigilance in the US. In Washington State, a resident has tested preliminarily positive for avian influenza, marking the first human case in 9 months. Meanwhile, in New Jersey, researchers have documented the nation’s first fatality linked to alpha-gal syndrome, which is a tick-borne meat allergy caused by the bite of the lone star tick.
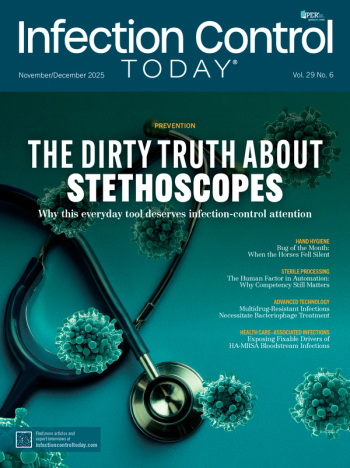
The November/December 2025 issue of Infection Control Today® dives into overlooked risks, breakthrough technologies, and the people driving innovation across IPC, EVS, and sterile processing. From bacteriophage therapy to burnout prevention, automation to UV regulation—it’s a powerful close to the year. Read the issue now: https://www.infectioncontroltoday.com/journals/infection-control-today #InfectionPrevention #Healthcare #InfectionControl #EVS #IPC #PatientSafety #ICT

After nearly a decade of research and regulatory review, the US Environmental Protection Agency (EPA) has determined that Micrillon, a polymer-based antimicrobial additive developed by UMF Corporation, is not a pesticide—clearing the way for new infection prevention applications. In this interview, UMF President George Clarke and Editorial Advisory Board member Heather Stoltzfus, MPH, RN, CIC, discussed how this rechargeable technology could redefine cleaning, sustainability, and surface safety across healthcare and hospitality settings.

Conversations about HIV and sexual health can still feel uncomfortable, but they don’t have to. In a candid interview, Hope & Help medical director Cariane Morales Matos, MD, explains why open, stigma-free discussions about HIV prevention and PrEP are essential for protecting teens, families, and communities.

I’ve known Monica and Tim forever, which is why their sepsis battles aren’t just “patient stories” to me. They’re a reminder that infection hides in ordinary days, and that vigilance, source control, and smart antibiotics save lives.
Infection prevention may be built on evidence, but it thrives on empathy. During a recent Infection Control Today roundtable, in this third installment, veteran infection preventionists shared how emotional intelligence, communication, and systems thinking—not just clinical expertise—define the profession’s future.
In a postpandemic health system, infection preventionists are hired for certifications but kept for soft skills. In this second installment of ICT's roundtable, veteran IPs chart the shift from task-doer to systems leader, calling for smarter staffing, structured onboarding, and relationship-first programs to beat burnout and turnover.
Infection prevention’s future will be won with mentorship, soft skills, and honest collaboration—not just guidelines. In a candid roundtable, veteran IPs shared how to steady first-year practitioners: pair them with real mentors, teach time management and tough conversations, and build cultures that value “let me confirm” over guesswork.

When a nationwide blood-culture bottle shortage squeezed hospitals, a Stanford-led team turned to machine learning by building and openly sharing tools that predict which patients are most likely to have bacteremia and when a culture can be safely deferred. The simplest version works as a quick bedside score, no new software required.

A Bangladesh research team unveiled a suitcase-sized, point-of-care test that detects Nipah virus from respiratory patients in about 30 minutes, showing accuracy comparable to RT-PCR, and designed to bring rapid diagnosis and outbreak control to rural, low-resource settings.

From hand-hygiene audits to the SHEA Board of Trustees, the professional path of Alexander Sundermann, DrPH, CIC, FAPIC, AL-CIP, traces the arc of modern infection prevention. The former hospital IP—now a University of Pittsburgh assistant professor—pairs frontline experience with genomic epidemiology to turn sequencing into outbreak-stopping action.

When Hurricane Helene flooded a North Carolina facility and sparked an IV fluid shortage, Duke’s stewardship network turned crisis into practice change—rapidly shifting eligible patients to highly bioavailable oral antibiotics and boosting PO use by 5.6% across participating hospitals.

At IDWeek in Atlanta, former CDC director Tom Frieden unveiled a crisp playbook for infection prevention—“See. Believe. Create.”—arguing it can help hospitals spot outbreaks sooner, reverse drug resistance, and drive HAIs toward zero. He paired the message with a 7-1-7 target: 7 days to find an outbreak, 1 to report, 7 to control.

What do schools need to prevent the spread of infectious diseases? Infection prevention experts and school staff in Nebraska present their collaboration at IDWeek2025.

California’s first locally acquired dengue case in 2023 triggered a rapid serosurveillance effort across Southern California—and IDWeek 2025 results suggest infections are underrecognized, with DENV-3 detected and widespread flavivirus cross-reactivity from West Nile virus complicating diagnosis.

Could Dollar General be Alabama’s next vaccination hub? At IDWeek 2025, John R. Bassler, MS, and colleagues showed that strategically pairing mobile clinics with DG stores could help close stubborn geographic vaccine gaps, especially in counties with higher social deprivation where traditional providers are scarce.

Hospital-wide sequencing of 8,567 Staphylococcus aureus isolates at NYU Langone revealed that many MRSA cases stem from tight community transmission networks—not in-hospital spread. Presented at IDWeek 2025, the work pinpoints distinct clusters (young MSM/substance-use networks, long-term care residents, and children) and urges IPC strategies that bridge hospital and community.

