After the Delta surge subsides, another surge is expected, possibly from the Mu variant. If Mu completely escapes immunity from vaccines and past infections, we must resort to stringent public health strategies.

KEVIN KAVANAGH, MD, is the founder of the patient advocacy group Health Watch USAsm, a member of the Infection Control Today's® Editorial Advisory Board, and a frequent contributor to Infection Control Today®.
Health Watch USAsm 2023 Webinar:
Long COVID: Patients, Workers & Society Webinar.
Webinar on Nov. 1, 2023. No charge for viewing or obtaining continuing education credits. CE planned and applied for ANCC Nursing, Physician Cat I ANA along with a number of other allied health professions.
Speakers Include:
Ambassador Deborah Birx, MD, past White House Coronavirus Coordinator. Presentation: "Impact of Long COVID on the United States. "
Pam Belluck, New York Times Reporter -- Presentation: "How Long COVID is affecting people's jobs and their needs at work."
Peter Hotez, MD, PhD, Dean of the National School of Tropical Medicine and Professor of Pediatrics and Molecular Virology & Microbiology at Baylor College of Medicine. will present on "Global Vaccines and Vaccinations: The Science vs The Anti-science."
Conference Objectives:
After attending the sessions about Long COVID, the participants will be able to:
* Describe the manifestations of Long COVID in different age groups.
* Discuss the different presentations of Long COVID.
* Identify the impacts of Long COVID on the healthcare workforce.
For more information go to: https://healthconference.org/
Agenda: https://www.healthconference.org/healthconference.org-files/2023Conference_downloads/_Agenda-3.pdf
Speaker's Bios: https://www.healthconference.org/healthconference.org-files/2023Conference_downloads/_Bios-Speakers-2023-HWUSA-Conference-9.pdf
Download Brochure: https://www.healthconference.org/healthconference.org-files/2023Conference_downloads/20231101-HWUSA_Brochure-5.pdf
Conference Registration - Space is limited:https://docs.google.com/forms/d/e/1FAIpQLSc3sHSOLLNNBwAXcDJlJo5NcuknMexia6H-0SsXJbjmK5YbFQ/viewform
Continuing Education:
Four AMA PRA Category 1 Continuing education credit hours have been approved for Physicians, Nursing Home Administrators and PA/Nurse Practitioners. The Kentucky Board of Nursing has approved the course for 4.8 credit hours. Through the corresponding Kentucky agency/board, Dentistry, Physical Therapy and EMS has been approved for 4 credit hours. Respiratory, Occupational Therapy, Social Work, Dietitian and Community Health Worker approval is pending.
American Nurses Credentialing Center (AANC) approval for 5 hours of continuing education is pending (Connecticut Nurses Association).
For more information, go to: https://healthconference.org/
After the Delta surge subsides, another surge is expected, possibly from the Mu variant. If Mu completely escapes immunity from vaccines and past infections, we must resort to stringent public health strategies.

In Beijing the total cases in an outbreak were reported to be less than 10. China used over 100 million tests to eradicate what would be classified as a very small outbreak by US standards.

In the Middle Ages a pandemic wiped out 50% of the world’s population. Presently we have a much higher population density, making us a feeding buffet for infectious disease…. If we do not follow the recommendations of modern science and public health, we are no better off than if we were living in the Middle Ages.
Herd immunity is no longer possible, the virus is mutating and likely has animal hosts. We must raise the bar on public health outcomes, not only focusing on deaths but also morbidity and long-hauler syndrome which can be all too common, even occurring with vaccine breakthrough infections.

A CDC investigation shows 2.3 times the number of reinfections with natural immunity compared to breakthrough infections in those who are vaccinated.

While not perfect, the mRNA vaccines do markedly reduce the chances of hospitalizations from critical disease and death. This is a huge plus.

Data collected by Britain’s Scientific Advisory Group for Emergencies, Japanese researchers, and the US Department of Agriculture paint a picture of a growing challenge.

Should older people get boosters? The data from Israel indicate that this needs to be given strong consideration in those above 60 years old who were fully vaccinated by the end of January.
Israeli announced today that it will begin offering a booster shot to its older citizens to try to stop the spread of the Delta variant. It is the first country in the world to make this move.
We need to have a paradigm shift in the way we view this virus, planning and implementing strategies to allow us to live with an endemic pathogen.

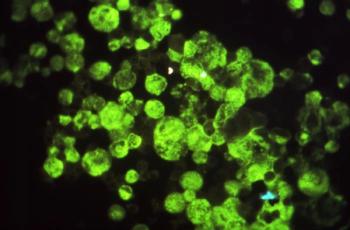
Beating back infection is a numbers game: viruses against antibodies. If the virus changes its armor so the antibodies cannot attach, it develops an advantage. However, it can also produce viruses which are more efficient at attaching to and invading cells, or simply just produce a lot more viruses, overwhelming the system.
Far too few have been fully vaccinated in the U.S.to ward off a run on our hospitals, and avoiding hospitalizations is an extremely low bar for public health, since 10% to 30% of the patients even with mild to moderate disease will develop long COVID.

As long as the immune escape variants are on the rise in the U.S. and less than half of our population is fully vaccinated, the best advice is to continue public health strategies.

Those of you who advocate reopening at the peril of those who are vaccine hesitant—letting nature decide the fate of the ill-informed—need to remember that survival is not the same as recovery.
Infection preventionists need to stress the importance of aerosolization with increased recommendations for N-95 masks and we all need to realize that a prerequisite of reopening a business, school or public venue should be safe ventilation.
What happens in India, or anywhere else in the world, doesn't stay there. The longer COVID-19 hangs around, the more chance it has of mutating into a variant that the vaccines won't stop.
If you work in a health care facility, you need to be vaccinated against SARS-CoV-2. If you choose not to become vaccinated, then you should choose not to be working in a health care setting.

Infection preventionists (IPs) are now faced with delivering a difficult message. It is much easier to advocate for vaccinations which prevent disease, than it is for vaccinations which lessen the severity of disease or reduces your chances of becoming infected.

The same mutation is found in the variant in Brazil but more disturbingly it is found in the New York variant.

SARS-CoV-2 is aerosolized. If a non-vaccinated person who is shedding the virus visits a vaccinated relative in a nursing home, he can easily spread the virus to all who reside in the facility.

The CMS update on when nursing home residents can have visitors raises grave concerns. The recommendation appears to assume that herd immunity is reached at 70%.

There needs to be a shift from droplet precaution standards to airborne spread standards and we need to invest in the safety of our frontline workers.

Frequent, (three times a week) screening of our athletes has been key to the opening of professional sports. Our students deserve the same safety precautions as professional athletes.
We need to have mandatory reporting of worker and patient acquisition of SARS-CoV-2 and the development of COVID-19 with metrics to provide us the most accurate estimate of cases so we can effectively plan and allocate resources.

The good news? The fact that 3 different viruses with 3 different lineages came up with the same mutation to evade natural immunity and the vaccines. And initial reports are that it only partially evades the vaccines.
Infection preventionists need to educate primary health providers on the importance of utilizing monoclonal antibodies to prevent hospitalizations from severe COVID-19.

Infection preventionists need to spread the message and articulate the uncertainties of this new variant of COVID-19. They need to emphasize that it is just not the old who are at risk and employ stricter containment measures.

We must treat this strain with the respect it deserves, but we must not panic. There is no doubt that increased infectivity equates with increases in deaths, but it does not mean the vaccines will not work.

V-Safe and VAERS are 2 monitoring systems for patients who are given a COVID-19 vaccine. Infection preventionists can play a vital role in educating about the strengths and drawbacks of each.

Infection preventionists are an important component of fostering trust in the healthcare system and need to actively articulate to both patients and on social media the need to be vaccinated and to follow public health advice.