As the COVID-19 pandemic continues to surge, it is unlikely that contact tracing within healthcare will become anything less than critical.
As the COVID-19 pandemic continues to surge, it is unlikely that contact tracing within healthcare will become anything less than critical.
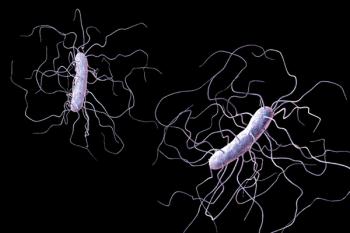
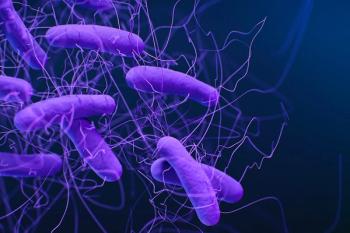
Coronavirus disease 2019 (COVID-19) has made hand hygiene all the rage. That’s too bad. Because hand hygiene doesn’t only help to slow the spread of COVID-19, but a slew of other dirty bugs, as well.

A telework-ready infection preventionist is an IP who continues to support their facility if they also end up in quarantine. Teleworking like so many other aspects of nursing is something we just needed to jump into. No training, no guidebook, no manual.

Charles P. Gerba, PhD: “Unfortunately, standard procedures for testing and registration by regulatory agencies of CADs (continuously active sanitizers or disinfectants) as disinfectants useful in preventing exposure to disease causing microorganism transmission has only taken place in recent years.”

Many factors make the isolation precautions for diseases like COVID-19 more complex than typical droplet or airborne definitions.
As the pandemic seems not to abate, patients will start to present to the hospital after delaying crucial primary and preventive care visits, meaning sicker non–COVID-19 infected patients, with the potential for increased CLABSI and CAUTI rates.

Jenny Hayes, MSN, RN, CIC: “Asking the patient to wear a mask, which is something that we do in our facility, can be challenging at that point, especially as labor progresses, and you’re to the point of pushing. That right there offers a set of unique challenges for both the patient and the staff in the room.”