
A rare Tennessee outbreak of Mycobacterium fortuitum revealed deep gaps in infection prevention at outpatient surgery centers—where oversight, staffing, and reporting often fall short.

A rare Tennessee outbreak of Mycobacterium fortuitum revealed deep gaps in infection prevention at outpatient surgery centers—where oversight, staffing, and reporting often fall short.

With staffing shortages and rising infection risks, the TEPHI 200-Series delivers accessible, high-impact training to empower healthcare professionals and strengthen infection prevention efforts nationwide.

Vatsala Srinivasa, MPH's, research uses genomic sequencing to track hospital transmission of respiratory viruses, revealing hidden links and highlighting the potential for improved infection prevention.
Noah Wald-Dickler, MD, FACP, discusses the safety and efficacy of oral transition therapy, challenges in antimicrobial stewardship, and evidence-based alternatives presented at SHEA 2024.

Danielle Zerr, MD, MPH, explains her presentations at SHEA 2024 about strategies for environmental pathogen control, the significance of patient-centered care in health care settings, and respiratory viruses in pediatric settings.
Tisha Mitsunaga, DrPH, ScM, discusses innovative approaches fostering collaboration between public health and healthcare facilities to combat multidrug-resistant organism (MDRO) spread.

A study presented at the Society for Healthcare Epidemiology of America (SHEA) conference evaluated adherence to laxative administration guidelines before CDI testing in Veteran Affairs (VA) hospitals and explored associated demographic and contextual factors.
Discover strategies for advocating infection prevention programs to the C-suite, ensuring resources, leadership support, and impactful outcomes.

In the infections the investigators examined, about 60% of the bacteria that cause these infections did have a carbapenemase gene. Did they find a mortality difference in those infections which did and didn’t?

Prescribers are presented with the optimal therapy challenges and achieving antibacterial stewardship.

With the focus of COVID-19, MRSA infections increased. How did the VA work to prevent this pathogen?
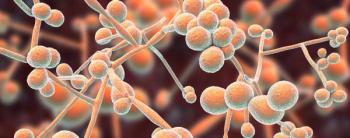
Candida auris environmental contamination is unlikely to be adequately controlled because re-contamination occurs within hours after disinfection.

A patient has a higher risk of infection of C difficile in a hospital bed that previously held a patient who also had C difficile.

Live attenuated influenza vaccine particles were released into a closed room to measure how many particles would get through the HVAC system.

However, a large-scale randomized controlled trial in health care is needed.

Patient pressure is a key driver of primary care providers to prescribe antibiotics.

Most information on SSI risk factors in the elderly is more than 10 years old.

Despite some benefits, challenges continue with implemented mitigation strategies for children and IPs.

IPs and other health care professionals needed to improvise. That improvisation led to investigations into how many times an N95 can be reused and still keep SARS- CoV-2 at bay.
Meri Pearson, MPH, CIC: “Infection preventionists still need to do those active audits to make sure that they’re actually seeing what’s happening at the bedside.”

Christina Yen, MD: “For any infection preventionists who are thinking about or are reviewing the need for VHP sometime in the future, just know that those colleagues that we’ve relied on this time around are going to be there and are going to be your partners in the VHP process.”

The lessons infection preventionists at the University of Mississippi Medical Center learned from an outbreak of respiratory illness at the facility’s NICU in 2019, were later used to help deal with the COVID-19 pandemic.
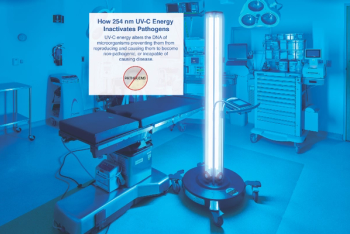
Ultraviolet light should be used in concert with traditional cleaning and disinfection procedures utilized by environmental services teams, study’s author maintains.

The infection prevention and business intelligence teams at Piedmont Healthcare put their heads together to streamline the process of tracking health care-acquired infections.

Emilie Bédard, PhD: “We worked in collaboration with infection prevention, environmental services…. We had a multi-disciplinary team to make sure that we would look at all aspects of this approach.”

The multidisciplinary team included NICU nurses, physicians, nurse practitioners and, perhaps most important of all, environmental services personnel. “We met with the environmental services staff, and we explained to them that this is a critical situation in the neonatal ICU. And this cannot spread more.”